| Posted on | Education
IUD Insights: Addressing Clinical Issues in Long-Term Contraceptive Methods
0
920 Views
Decades of seeking convenient contraception yielded diverse methods, each with unique strengths and limitations, shaping reproductive health strategies. Among these, the intrauterine device (IUD) stands out for its long-acting, reversible nature, offering years of protection with minimal user intervention.
Yet, despite its undeniable efficacy, the clinical landscape surrounding IUDs remains shrouded in a veil of incomplete information and lingering concerns.
In this article, we aim to illuminate this often-overlooked terrain by exploring the intricacies of IUD insertion, potential complications, and strategies for optimal management.
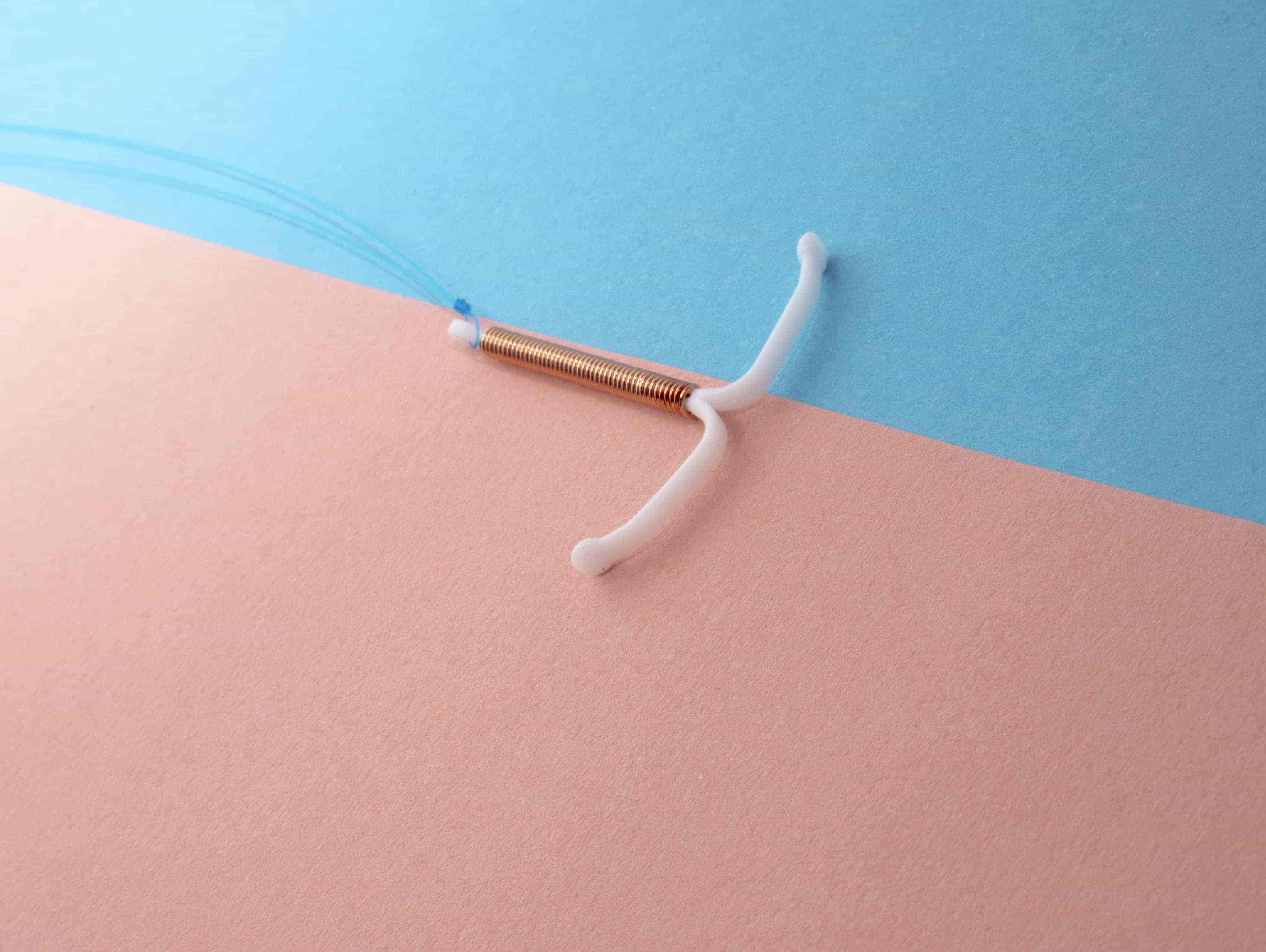
Image Credit (unsplash)
Understanding the Mechanism of IUDs
Despite their simple design, IUDs operate through a sophisticated interplay of local and systemic effects. They function via hormonal and non-hormonal mechanisms, offering a dual approach to contraception with distinct physiological impacts.
Hormonal IUDs work by releasing a low-dose progestin, often levonorgestrel. This progestin thickens cervical mucus, making it difficult for sperm to enter the uterus, and also thins the uterine lining, hindering embryo implantation.
Copper-based non-hormonal devices release copper ions in the uterine cavity, creating a hostile environment for sperm and impeding motility and viability. This, along with an inflammatory response triggered by their presence, significantly reduces the chances of fertilization. This dual-action approach positions these gadgets as highly reliable contraceptives.
Data from Planned Parenthood indicates that both hormonal and copper IUDs boast an efficacy rate exceeding 99%. It underscores the robustness of these gadgets as a contraceptive choice. Optimizing their use requires understanding the interplay of mechanisms and individual factors to enhance efficacy in clinical practice.
Clinical Challenges in IUD Placement
While IUDs stand as a stalwart in long-term contraceptive methods, their successful deployment is not without clinical challenges. Their placement involves a delicate procedure that demands precision and expertise, posing potential hurdles for both healthcare providers and patients.
One prominent challenge is the risk of uterine perforation during insertion, emphasizing the need for skilled practitioners and careful patient selection.
Also, anatomical differences and medical history impact their insertion, introducing complexity to the procedure for healthcare providers and patients alike. Insertion pain may pose clinical concerns, impacting patient adherence to this contraceptive method and highlighting the need for enhanced comfort measures.
Addressing these challenges necessitates a nuanced understanding of patient-specific factors, advancements in insertion techniques, and ongoing professional training.
Managing Side Effects and Complications
While IUDs are generally well-tolerated, they can occasionally cause side effects and complications. Understanding and addressing these concerns is key to ensuring a smooth and positive experience.
Common side effects after the insertion include mild cramping and discomfort, alleviated by over-the-counter pain relievers and warm compresses. Hormonal IUDs may impact menstrual patterns, lightening or shortening periods, while copper ones may initially cause heavier bleeding.
Mood changes and acne are potential effects, necessitating communication with healthcare providers for symptom tracking and potential adjustments.
Less common complications include pelvic inflammatory disease (PID), which is a rare but serious infection not heightened by these gadgets. Timely diagnosis and treatment are vital. IUD expulsion, sometimes unnoticed, underscores the importance of regular self-checks for strings and prompt follow-up if absent. In rare cases, uterine perforation during insertion necessitates immediate removal.
News Medical Life Sciences reported that among women with these devices, about 5% experienced expulsion, and 0.1% faced uterine perforation. It highlights the overall safety and low risk of serious complications associated with them. Remember, vigilance and swift responses are crucial in managing these less common but potentially serious complications associated with intrauterine devices.
Infection Risks and Prevention
While these devices boast impressive contraceptive efficacy, they do carry a small risk of infection, particularly in the short period after insertion. Pelvic inflammatory disease (PID) is the most serious concern, although its prevalence is fortunately low. MedicalNewsToday reports that while pelvic inflammatory disease (PID) can result from their use, the risk is exceedingly low. Noted incidence is less than 1%.
Understanding the potential risks and implementing preventive measures helps ensure a safe and successful experience. Amidst the myriad benefits, the specter of infection remains a notable concern. Despite the overall effectiveness of copper-containing Paragard IUDs, isolated cases report infections, prompting nuanced discussions on associated risks.
Lawsuits against Paragard's manufacturer, Teva Pharmaceuticals, raise concerns over potential infection risks, notably associated with breakage during removal procedures.
The Paragard lawsuit contends the company's failure to adequately warn the users about potential risks associated with the device. The plaintiffs seek compensation for related injuries, encompassing medical costs, pain, and suffering incurred due to the device.
TorHoerman Law notes the consolidation of Paragard lawsuits into an MDL in the US District Court for the Northern District of Georgia. If you or a loved one faced complications after using a Paragard device, you may be eligible for a Paragard lawsuit.
Expulsion and Displacement Concerns
In the dominion of long-term contraception, these devices pose concerns about expulsion and displacement. Despite their effectiveness, unintended expulsion or displacement raises clinical concerns. These issues involve the device being pushed out or shifting from its optimal position.
Imagine your gadget taking an unplanned vacation outside the uterus. That's expulsion. It occurs when it partially or completely dislodges from its rightful position. Unlike expulsion, displacement happens when the device stays within the uterus but shifts from its optimal position.
Addressing expulsion and displacement requires vigilance post-insertion, patient education on recognizing signs, and consideration of individual risk factors.
Long-Term Effectiveness and Continuation
Beyond their initial efficacy, IUDs shine in their long-lasting protection. With a lifespan of several years, depending on the type, they offer years of worry-free contraception, minimizing the need for frequent intervention. This sustained effectiveness is a significant public health advantage, as continuation rates are crucial in preventing unintended pregnancies.
Nemours TeensHealth notes that the copper intrauterine device is instantly effective and lasts up to 10 years, offering long-term contraception. Progestin ones provide effective contraception for 3 to 6 years, depending on the brand. It translates to years of reliable protection with minimal user intervention, significantly reducing the risk of unintended pregnancy. While they offer long-term protection, healthcare providers can remove them at any time.
Emerging Technologies and Innovations
In the ever-evolving landscape of long-term contraceptive methods, emerging technologies and innovations are shaping the future of intrauterine devices. Recent advancements delve into refining insertion techniques, improving user experience, and addressing specific clinical concerns. Notably, novel materials and designs aim to enhance comfort and reduce the likelihood of expulsion or displacement.
Also, integrating smart technologies into contraceptives enables real-time monitoring and personalized feedback, enhancing a proactive and user-centric approach to care.
Ongoing innovations blend data-driven insights and advanced designs, reshaping long-term contraceptives and enhancing safety, efficacy, and user experience.
Navigating the Future of Contraception with IUD Insights
This article discloses the multifaceted landscape clinicians and individuals navigate within the dynamic sphere of long-term contraceptive methods, especially IUDs. In conclusion, these devices, despite challenges, emerge resilient as pivotal players in advancing reproductive health solutions.
Built on data-driven insights and a commitment to addressing clinical intricacies, the future of these devices promises continued advancements and effectiveness
